Preimplantation genetic testing for monogenic diseases (PGT-M) is a method that allows for the selection of a healthy embryo without a specific genetic burden.
For whom the method is suitable
For all couples with a genetic burden in the family who are planning a baby
Approximate price
You can find out the current terms for the reimbursement of preimplantation examinations by consulting your doctor. For more detailed information about prices, see our price list.
How it works
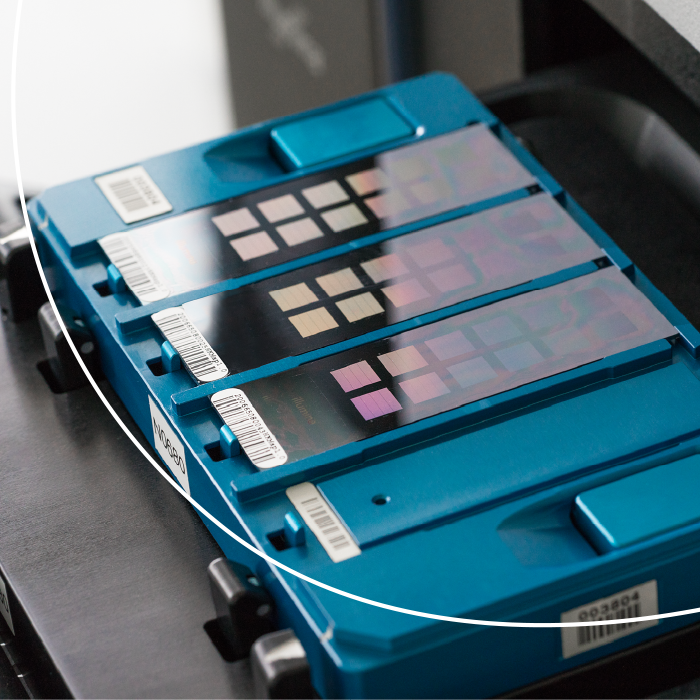
We take a few cells from the embryos on the 5th to 6th days of their development. We then freeze the embryos and work only with those harvested cells. We perform Karyomapping or OneGene PGT tests in our genetic laboratory. We are able to rule out virtually any rare hereditary disease.
Genetic testing of embryos takes about 3 weeks. At the end, we get information about the genetic make-up of the embryos we have tested, so we know for sure which are suitable for transfer. The transfer can take place in the next cycle.